Obstructive sleep apnea
is the most common sleep-related breathing disorder
Risk Factors
Anyone can develop obstructive sleep apnea. However, certain factors put you at increased risk, including:
Excess weight
Most but not all people with obstructive sleep apnea are overweight. Fat deposits around the upper airway can obstruct breathing. Medical conditions that are associated with obesity, such as hypothyroidism and polycystic ovary syndrome, also can cause obstructive sleep apnea.
Older age
The risk of obstructive sleep apnea increases as you age but appears to level off after your 60s and 70s.
Narrowed airway
- You might inherit naturally narrow airways. Or your tonsils or adenoids might become enlarged and block your airway.
High blood pressure (hypertension)
Obstructive sleep apnea is relatively common in people with hypertension.
Chronic nasal congestion
Obstructive sleep apnea occurs twice as often in those who have consistent nasal congestion at night, regardless of the cause. This may be due to narrowed airways.
Smoking
People who smoke are more likely to have obstructive sleep apnea.
Diabetes
Obstructive sleep apnea might be more common in people with diabetes.
Sex
In general, men are twice or three times as likely as premenopausal women to have obstructive sleep apnea. The frequency of obstructive sleep apnea increases in women after menopause.
A family history of sleep apnea
Having family members with obstructive sleep apnea might increase your risk.
Asthma
Research has found an association between asthma and the risk of obstructive sleep apnea.
Symptoms
Signs and symptoms of obstructive sleep apnea include:
- Excessive daytime sleepiness
- Loud snoring
- Observed episodes of stopped breathing during sleep
- Abrupt awakenings accompanied by gasping or choking
- Awakening with a dry mouth or sore throat
- Morning headache
- Difficulty concentrating during the day
- Mood changes, such as depression or irritability
- High blood pressure
- Decreased libido
When to see a doctor
Consult a medical professional if you have, or if your partner observes, the following:
- Snoring loud enough to disturb your sleep or that of others
- Waking up gasping or choking
- Pausing in your breathing during sleep
- Having excessive daytime drowsiness, which may cause you to fall asleep while working, watching television or even driving a vehicle
Snoring doesn't necessarily indicate something potentially serious, and not everyone who snores has obstructive sleep apnea.
Be sure to talk to your doctor if you snore loudly, especially if your snoring is interrupted by periods of silence. With obstructive sleep apnea, snoring usually is loudest when you sleep on your back, and it quiets when you turn on your side.
Ask your doctor about any sleep problem that leaves you chronically fatigued, sleepy and irritable. Excessive daytime drowsiness may be due to other disorders, such as narcolepsy.
Causes
Obstructive sleep apnea occurs when the muscles in the back of your throat relax too much to allow normal breathing. These muscles support structures including the back of the roof of your mouth (soft palate), the triangular piece of tissue hanging from the soft palate (uvula), the tonsils and the tongue.
When the muscles relax, your airway narrows or closes as you breathe in, hampering your breathing for 10 seconds or longer. This can lower the level of oxygen in your blood and cause a buildup of carbon dioxide.
Your brain senses this impaired breathing and briefly rouses you from sleep so that you can reopen your airway. This awakening is usually so brief that you don't remember it.
You can awaken with shortness of breath that corrects itself quickly, within one or two deep breaths. You might make a snorting, choking or gasping sound.
This pattern can repeat itself five to 30 times or more each hour, all night long. These disruptions impair your ability to reach the deep, restful phases of sleep, and you'll probably feel sleepy during your waking hours.
People with obstructive sleep apnea might not be aware of their interrupted sleep. Many people with this type of sleep apnea don't realize they haven't slept well all night.
Complications
Obstructive sleep apnea is considered a serious medical condition. Complications can include:
Daytime fatigue and sleepiness. Because of a lack of restorative sleep at night, people with obstructive sleep apnea often have severe daytime drowsiness, fatigue and irritability. They might have difficulty concentrating and find themselves falling asleep at work, while watching TV or even when driving. This can put them at higher risk of work-related accidents.
Children and young people with obstructive sleep apnea might do poorly in school and commonly have attention or behavior problems.
Cardiovascular problems. Sudden drops in blood oxygen levels that occur during obstructive sleep apnea increase blood pressure and strain the cardiovascular system. Many people with obstructive sleep apnea develop high blood pressure (hypertension), which can increase the risk of heart disease.
The more severe the obstructive sleep apnea, the greater the risk of coronary artery disease, heart attacks, heart failure and strokes.
Obstructive sleep apnea increases the risk of abnormal heart rhythms (arrhythmias), which can lower blood pressure. If there's underlying heart disease, these repeated multiple episodes of arrhythmias could lead to sudden death.
Complications with medications and surgery. Obstructive sleep apnea is also a concern with certain medications and general anesthesia. These medications, such as sedatives, narcotic analgesics and general anesthetics, relax your upper airway and can worsen your obstructive sleep apnea.
If you have obstructive sleep apnea, having major surgery, especially after being sedated and lying on your back, can worsen breathing problems. People with obstructive sleep apnea might be more prone to complications after surgery.
Before you have surgery, tell your doctor if you have obstructive sleep apnea or symptoms related to the condition. Your doctor might want you tested for obstructive sleep apnea before surgery.
- Eye problems. Some research has found a connection between obstructive sleep apnea and certain eye conditions, such as glaucoma. Eye complications can usually be treated.
- Sleep-deprived partners. Loud snoring can keep those around you from getting good rest and eventually disrupt your relationships. Some partners choose to sleep in another room.
People with obstructive sleep apnea may also complain of memory problems, morning headaches, mood swings or depression, and a need to urinate frequently at night.
Obstructive sleep apnea might be a risk factor for COVID-19. People with obstructive sleep apnea have been found to be at higher risk for developing a severe form of COVID-19 and needing hospital treatment than those who don't have obstructive sleep apnea.
Lifestyle and home remedies
In many cases, self-care may be the most appropriate way for you to deal with obstructive sleep apnea. Try these tips:
- Lose weight. If you're overweight or obese, even a moderate loss of excess weight may help relieve constriction of your airway. Losing weight can also improve your health and quality of life and might reduce your daytime sleepiness.
- Exercise. Exercising, such as aerobic exercise and strength training, can help improve your condition. Aim to exercise about 150 minutes a week, and generally try to exercise most days of the week.
- Avoid alcohol and medications such as anti-anxiety drugs and sleeping pills. Alcohol, some anti-anxiety medications, and some sleeping pills can worsen obstructive sleep apnea and sleepiness.
Sleep on your side or stomach rather than on your back. Sleeping on your back can cause your tongue and soft palate to rest against the back of your throat and block your airway.
To prevent sleeping on your back, try sewing a tennis ball in the back of your pajama top or place pillows behind you while you sleep on your side.
- Keep your nasal passages open while you sleep. If you have congestion, use a saline nasal spray to help keep your nasal passages open. Talk to your doctor about using nasal decongestants or antihistamines, because some medications may be recommended for only short-term use.
What to expect from your doctor
A key part of the evaluation of obstructive sleep apnea is a detailed history, meaning your doctor will ask you many questions. These may include:
- When did you first notice symptoms?
- Have your symptoms been off and on, or do you always have them?
- Do you snore? If so, does your snoring disrupt anyone else's sleep?
- Do you snore in all sleep positions or just when sleeping on your back?
- Do you ever snore, snort, gasp or choke yourself awake?
- Has anyone seen you stop breathing during sleep?
- How refreshed do you feel when you wake up? Are you tired during the day?
- Do you have a headache or dry mouth when you awaken?
- Do you doze off or have trouble staying awake while sitting quietly or driving?
- Do you nap during the day?
- Do you have family members with sleep problems?
What you can do in the meantime
- Try to sleep on your side. Most forms of obstructive sleep apnea are milder when you sleep on your side.
- Avoid drinking alcohol close to bedtime. Alcohol worsens obstructive sleep apnea.
- If you're drowsy, avoid driving. If you have obstructive sleep apnea, daytime sleepiness can put you at higher risk of motor vehicle accidents. To be safe, schedule rest breaks. If a close friend or family member ever tells you that you appear sleepier than you feel, try to avoid driving.
Common Treatments

Continuous positive airway pressure (CPAP
To eliminate snoring and prevent sleep apnea, your doctor may recommend a device called a continuous positive airway pressure (CPAP) machine. A CPAP machine delivers just enough air pressure to a mask to keep your upper airway passages open, preventing snoring and sleep apnea.

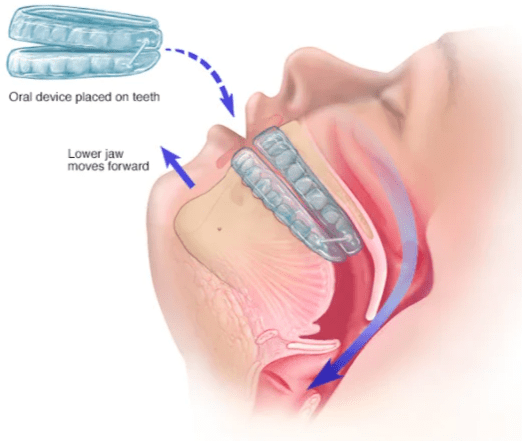
Oral device
An oral device is placed on the teeth and is designed to keep your throat open by holding your tongue and lower jaw forward.

Airway stimulation system
An impulse generator is implanted in the chest and stimulates the nerve that controls tongue movements.
Upper jaw advancement
Upper jaw advancement surgery involves moving the jaw to reduce the risk of obstruction.
Surgical removal of tissue
Uvulopalatopharyngoplasty (UPPP) is a procedure in which your doctor removes tissue from the back of your mouth and top of your throat. Your tonsils and adenoids may be removed as well. UPPP usually is performed in a hospital and requires a general anesthetic.
Surgical opening in the neck (tracheostomy)
You may need this form of surgery if other treatments have failed and you have severe, life-threatening obstructive sleep apnea.
During a tracheostomy, your surgeon makes an opening in your neck and inserts a metal or plastic tube through which you breathe. Air passes in and out of your lungs, bypassing the blocked air passage in your throat.
Other types of surgery may help reduce snoring and sleep apnea by clearing or enlarging air passages, including:
- Nasal surgery to remove polyps or straighten a crooked partition between your nostrils (deviated septum)
- Surgery to remove enlarged tonsils or adenoids

Sleep Vigil ensures your interventions are effective by making it easy to review relevant physiological patient data
Sign Up for early access today
Sleep Vigil © 2021 Powered By: GatherMed